Herpes Zoster Ophthalmicus
Herpes Zoster Ophthalmicus (HZO) refers to the involvement of the ophthalmic branch (V1) of the trigeminal nerve by the Varicella-Zoster Virus (VZV). This virus belongs to the Herpesviridae family and is responsible for causing varicella (chickenpox) during the initial infection in childhood.
Herpes Zoster Ophthalmicus
Herpes Zoster Ophthalmicus (HZO) refers to the involvement of the ophthalmic branch (V1) of the trigeminal nerve by the Varicella-Zoster Virus (VZV). This virus belongs to the Herpesviridae family and is responsible for causing varicella (chickenpox) during the initial infection in childhood. After the primary infection, the virus remains latent for a long period within the sensory ganglia of the body, particularly in the trigeminal ganglion.
Reactivation of the Varicella-Zoster Virus typically occurs due to a decline in the immune system, which may result from aging, immunosuppressive diseases, or certain medications. Upon reactivation, the virus travels from neurons to the skin and adjacent tissues, leading to painful cutaneous lesions as well as involvement of various ocular and periocular structures.
Involvement of any branch of the trigeminal nerve can lead to zoster in the respective region, but when the ophthalmic branch (V1) is affected, there is a risk of injury to the eyelids, conjunctiva, cornea, sclera, iris, uvea, and even the retina and optic nerve. This condition can result in severe and sometimes permanent ocular complications, underscoring the importance of early diagnosis, prompt treatment, and meticulous monitoring.
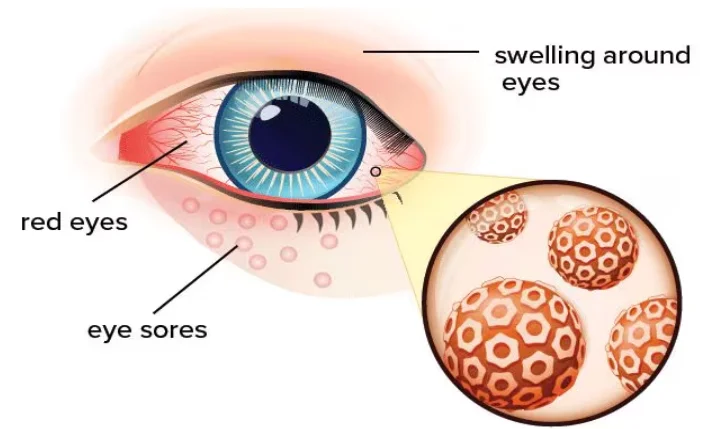
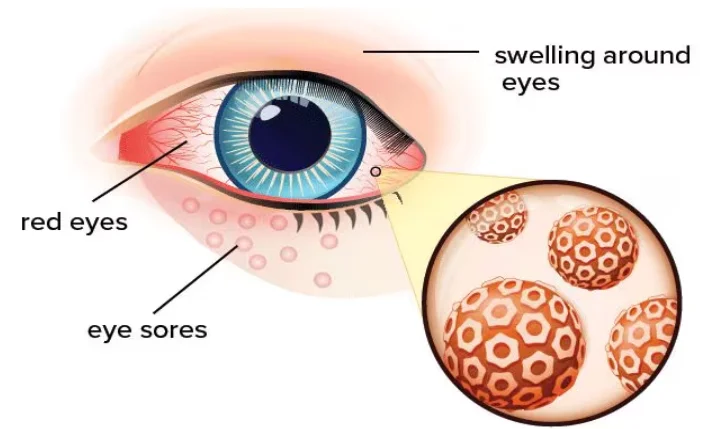
Herpes Zoster Ophthalmicus may present with systemic symptoms and vesicular skin lesions on the forehead and around the eye, accompanied by a spectrum of ocular problems such as conjunctivitis, keratitis, uveitis, and even neuro-ophthalmic and retinal complications. Therefore, HZO is not only considered an ophthalmic emergency but also one of the most significant complications of herpes zoster in adults and the elderly.
Epidemiology
Herpes Zoster Ophthalmicus accounts for approximately 10 to 20 percent of all cases of herpes zoster. This condition predominantly affects individuals over the age of 50, and the presence of underlying factors such as diabetes or immunosuppressive diseases increases the risk of developing the disease.
Clinical Symptoms
“Prodromal symptoms include pain, burning, or tingling in the forehead, eyelid, and periorbital area, emerging days before rash onset. Vesicular eruptions follow along the ophthalmic division. Involvement of the tip of the nose (Hutchinson’s sign) is a marker for increased ocular complication risk. Ocular involvement may manifest as conjunctivitis, episcleritis, keratitis (superficial or deep), anterior uveitis, scleritis, and rarely, retinitis or optic neuritis. Other symptoms include decreased vision, photophobia, lacrimation, and eye pain.”
General Management and Follow-up
The primary goal of management in patients with ocular surface lesions is to prevent secondary infection. Careful examination is necessary to confirm or rule out inflammation in various layers of the eye, and to initiate appropriate treatment if required. If skin lesions are the only clinical manifestation, follow-up should be conducted to monitor for the possible onset of ocular involvement and promptly initiate treatment if needed.
Medical Management
Supportive care, pain control, and management of inflammation are the mainstays of therapy. When internal ocular structures are involved, antiviral and anti-inflammatory treatment should be administered at the discretion of a specialist. Intraocular pressure must be regularly monitored and, if elevated, appropriately managed. For severe or neuropathic pain, targeted therapies are provided under physician supervision to decrease the risk of post-herpetic neuralgia.
Medical Follow-up
The interval of clinical follow-up depends on the extent and type of ocular involvement. During the acute phase, evaluations are generally recommended every 1 to 7 days; after this period, follow-ups at intervals of 3 to 12 months are advised to monitor for late complications such as elevated intraocular pressure, cataract, or corneal scarring. In selected cases, prophylactic medical therapy may be considered to reduce the risk of recurrence.
Surgical Management
If the transparency or structural integrity of the cornea is severely compromised, corneal transplantation becomes necessary. Additional surgical interventions—including surgery for the retina or intraocular pressure—are indicated only if the condition does not respond to medical treatment and as determined by a subspecialist. If cataract develops secondary to inflammation or its treatment, cataract surgery can be considered, but only after disease control is achieved.
Postoperative Follow-up
After surgery, it is crucial to closely monitor for significant inflammation, as this can be more common and severe in patients with a history of viral eye disease. Prophylactic antiviral therapy and anti-inflammatory medications should be continued as directed by the treating physician to minimize the risk of recurrence.
Prevention
Nowadays, the shingles vaccine (Shingrix) is recommended for adults over the age of 50 or for immunocompromised individuals, with an efficacy exceeding 90%. This vaccine significantly reduces the incidence of shingles and postherpetic neuralgia (Dooling KL, MMWR 2018)[2]. Strengthening population immunity, especially as natural exposure to VZV decreases, has become increasingly important.
Complications and Outcomes
Complications include postherpetic neuralgia (the most common long-term complication), vision loss, corneal involvement, chronic uveitis, and, according to some studies, an increased risk of stroke.
Sources:
StatPearls Publishing. Herpes Zoster Ophthalmicus [Updated 2024].
StatPearls – Herpes Zoster Ophthalmicus, 2024
Farooq AV, Shukla D, Chodosh J. Viral Conjunctivitis. StatPearls Publishing. Updated 2024.