If you have dryness, pain or redness in the eye area when you wake up, you most likely have dry eyes.
Dry eyes
Overview
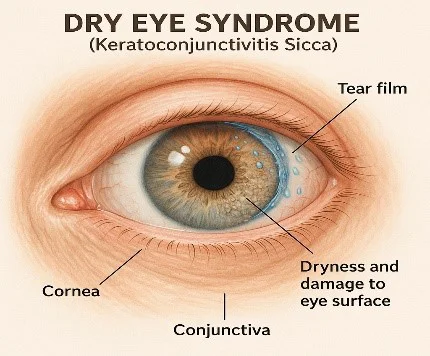
Dry eye disease is a common condition that occurs when your tears aren't able to provide adequate lubrication for your eyes. Tears can be inadequate and unstable for many reasons. For example, dry eyes may occur if you don't produce enough tears or if you produce poor-quality tears. This tear instability leads to inflammation and damage of the eye's surface.
Dry eyes feel uncomfortable. If you have dry eyes, your eyes may sting or burn. You may experience dry eyes in certain situations, such as on an airplane, in an air-conditioned room, while riding a bike or after looking at a computer screen for a few hours.
Treatments for dry eyes may make you more comfortable. These treatments can include lifestyle changes and eye drops. You'll likely need to take these measures indefinitely to control the symptoms of dry eyes.
Symptoms
Signs and symptoms, which usually affect both eyes, may include:
- A stinging, burning or scratchy sensation in your eyes
- Stringy mucus in or around your eyes
- Sensitivity to light
- Eye redness that progresses through the day
- A sensation of having something in your eyes
- Difficulty wearing contact lenses
- Difficulty with nighttime driving
- Watery eyes, which is the body's response to the irritation of dry eyes
- Blurred vision or eye fatigue
Causes
Dry eyes are caused by a variety of reasons that disrupt the healthy tear film. Your tear film has three layers: fatty oils, aqueous fluid and mucus. This combination usually keeps the surface of your eyes lubricated, smooth and clear. Problems with any of these layers can cause dry eyes.
Reasons for tear film dysfunction are many, including hormone changes, autoimmune disease, inflamed eyelid glands or allergic eye disease. For some people, the cause of dry eyes is decreased tear production or increased tear evaporation.
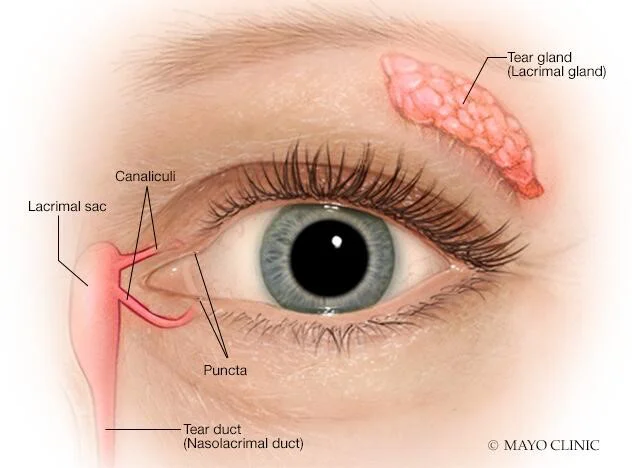
Tear glands and tear ducts
The tear glands located above each eyeball, called the lacrimal glands, continuously supply tear fluid that's wiped across the surface of your eye each time you blink your eyelids. Excess fluid drains through the tear ducts into the nose.
Decreased tear production
Dry eyes can occur when you're unable to produce enough liquid tears. Common causes of decreased tear production include:
- Aging
- Certain medical conditions including Sjogren's syndrome, allergic eye disease, rheumatoid arthritis, lupus, scleroderma, sarcoidosis, thyroid disorders or vitamin A deficiency
- Certain medicines, including antihistamines, decongestants, hormone replacement therapy, antidepressants, and medicines for high blood pressure, acne, birth control and Parkinson's disease
- Corneal nerve desensitivity caused by contact lens use, nerve damage or laser eye surgery, though symptoms of dry eyes related to this procedure are usually temporary
Increased tear evaporation
The oil film produced by small glands on the edge of your eyelids (meibomian glands) might become clogged. Blocked meibomian glands are more common in people with rosacea or other skin disorders.
Common causes of increased tear evaporation include:
- Posterior blepharitis (meibomian gland dysfunction)
- Blinking less often, which tends to occur with certain conditions, such as Parkinson's disease; or when you're concentrating during certain activities, such as while reading, driving or working at a computer
- Eyelid problems, such as the lids turning outward (ectropion) and the lids turning inward (entropion)
- Eye allergies
- Preservatives in topical eye drops
- Wind, smoke or dry air
- Vitamin A deficiency
Risk factors
Factors that make it more likely that you'll experience dry eyes include:
- Being older than 50. Tear production tends to diminish as you get older. Dry eyes are more common in people over 50.
- Being a woman. A lack of tears is more common in women, especially if they experience hormonal changes due to pregnancy, using birth control pills or menopause.
- Eating a diet that is low in vitamin A, which is found in liver, carrots and broccoli, or low in omega-3 fatty acids, which are found in fish, walnuts and vegetable oils.
- Wearing contact lenses or having a history of refractive surgery.
Complications
People who have dry eyes may experience these complications:
- Eye infections. Your tears protect the surface of your eyes from infection. Without adequate tears, you may have an increased risk of eye infection.
- Damage to the surface of your eyes. If left untreated, severe dry eyes may lead to eye inflammation, abrasion of the corneal surface, corneal ulcers and vision loss.
- Decreased quality of life. Dry eyes can make it difficult to perform everyday activities, such as reading.
Prevention
If you experience dry eyes, pay attention to the situations that are most likely to cause your symptoms. Then find ways to avoid those situations in order to prevent your dry eyes symptoms. For instance:
- Avoid air blowing in your eyes. Don't direct hair dryers, car heaters, air conditioners or fans toward your eyes.
- Add moisture to the air. In winter, a humidifier can add moisture to dry indoor air.
- Consider wearing wraparound sunglasses or other protective eyewear. Safety shields can be added to the tops and sides of eyeglasses to block wind and dry air.
- Take eye breaks during long tasks. If you're reading or doing another task that requires visual concentration, take periodic eye breaks. Close your eyes for a few minutes. Or blink repeatedly for a few seconds to help spread your tears evenly over your eyes.
- Be aware of your environment. The air at high altitudes, in desert areas and in airplanes can be extremely dry. When spending time in such an environment, it may be helpful to frequently close your eyes for a few minutes at a time to minimize evaporation of your tears.
- Working at a computer. reading or watching television can dry your eyes out. This is because you don’t blink as often as you normally do. Take breaks every 10 minutes, give your eyes a rest and try to blink more frequently to help your eyes regain some of the moisture they've lost.
- Position your computer screen below eye level. If your computer screen is above eye level, you'll open your eyes wider to view the screen. Position your computer screen below eye level so that you won't open your eyes as wide. This may help slow the evaporation of your tears between eye blinks.
- Stop smoking and avoid smoke. If you smoke, quit-smoking. If you don't smoke, stay away from people who do. Smoke can worsen dry eyes symptoms.
- Use artificial tears regularly. If you have chronic dry eyes, use eye drops even when your eyes feel fine to keep them well lubricated.
- Medications. If you have symptoms of dry eyes and take medication, read the label. Some drugs, such as antihistamines, beta-blockers, and some antidepressants, can affect your tears and dry out your eyes. Talk with your doctor to find out if this is a problem for you.
Diagnosis
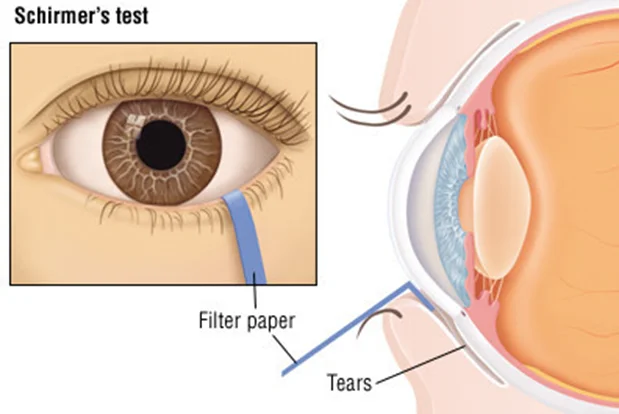
Tests and procedures that may be used to determine the cause of your dry eyes include:
- A comprehensive eye exam. An eye exam that includes a complete history of your overall health and your eye health can help your eye care specialist diagnose the cause of your dry eyes.
- A test to measure the volume of your tears. Your eye care specialist may measure your tear production using the Schirmer tear test. In this test, blotting strips of paper are placed under your lower eyelids. After five minutes your eye care specialist measures the amount of strip soaked by your tears.
-
- A test to determine the quality of your tears. Other tests use special dyes in eye drops to determine the surface condition of your eyes. Your eye care specialist looks for staining patterns on the corneas and measures how long it takes before your tears evaporate.
- A tear osmolarity test. This type of test measures the composition of particles and water in your tears. With dry eye disease, there will be less water in your eyes.
- Tear samples to look for markers of dry eye disease, including elevated matrix metalloproteinase-9 or decreased lactoferrin.
-
Treatment
For most people with occasional or mild dry eye symptoms, it's enough to regularly use nonprescription eye drops, also called artificial tears. If your symptoms are persistent and more serious, you have other options. What you do depends on what's causing your dry eyes.
Some treatments focus on reversing or managing a condition or factor that's causing your dry eyes. Other treatments can improve your tear quality or stop your tears from quickly draining away from your eyes.
Treating the underlying cause of dry eyes
In some cases, treating an underlying health issue can help clear up the signs and symptoms of dry eyes. For instance, if a medication is causing your dry eyes, your eye care specialist may recommend a different medicine that doesn't cause that side effect.
Medications
Prescription medicines used to treat dry eyes include:
- Medicines to reduce eyelid inflammation. Inflammation along the edge of your eyelids can keep oil glands from secreting oil into your tears. Your eye care specialist may recommend antibiotics to reduce inflammation. Antibiotics for dry eyes are usually taken by mouth, though some are used as eye drops or ointments.
- Eye drops to control cornea inflammation. Inflammation on the surface of your eyes (cornea) may be controlled with prescription eye drops that contain the immune-suppressing medicine cyclosporine or corticosteroids. Corticosteroids are not ideal for long-term use due to possible side effects.
- Tear-stimulating medicines. Medicines called cholinergics (pilocarpine) help increase tear production. Possible side effects include sweating.
- Eye drops made from your own blood. These are called autologous blood serum drops. They may be an option if you have severe dry eye symptoms that don't respond to any other treatment. To make these eye drops, a sample of your blood is processed to remove the red blood cells and then mixed with a salt solution.
-
Other procedures
Other procedures that may be used to treat dry eyes include:
- Closing your tear ducts to reduce tear loss. Your eye care specialist may suggest this treatment to keep your tears from leaving your eye too quickly. This can be done by partially or completely closing your tear ducts, which normally serve to drain tears away.
- Using special contact lenses. Some people with severe dry eyes may opt for special contact lenses that protect the surface of the eyes and trap moisture. These are called scleral lenses or bandage lenses.
- Unblocking oil glands. Warm compresses or eye masks used daily can help clear up blocked oil glands. A thermal pulsation device is another way to unclog the oil glands, but it is unclear whether this method provides any advantage over warm compresses.
- Using light therapy and eyelid massage. A technique called intense-pulsed light therapy followed by massage of the eyelids may help people with severe dry eyes.
-
Self care
You may be able to manage your dry eyes with frequent eyelid washing and use of nonprescription eye drops or other products that help lubricate your eyes. If your condition is long term (chronic), use eye drops even when your eyes feel fine to keep them well lubricated.
Selecting and using nonprescription products for dry eyes
A variety of nonprescription products for dry eyes are available, including eye drops, also called artificial tears. Talk with your eye care specialist about which might be best for you.
Artificial tears may be all you need to control mild dry eye symptoms. Some people need to put drops in several times a day, and some use them only once a day.
Consider these factors when selecting a nonprescription product:
- Preservative vs. nonpreservative drops. Preservatives are added to some eye drops to prolong shelf life. You can use eye drops with preservatives up to four times a day. But using the preservative drops more often can cause eye irritation.
-
Nonpreservative eye drops come in packages that contain multiple single-use vials. After you use a vial, you throw it away. If you rely on eye drops more than four times a day, nonpreservative drops are safe.
- Drops vs. ointments. Lubricating eye ointments coat your eyes, providing longer lasting relief from dry eyes. But these products are thicker than eye drops and can cloud your vision. For this reason, ointments are best used just before bedtime. Eye drops can be used at any time and won't interfere with your vision.
- Drops that reduce redness. It's best to avoid these as your solution for dry eyes, as prolonged use can cause irritation.
-
Washing your eyelids to control inflammation
For people with blepharitis and other conditions that cause eyelid inflammation that blocks the flow of oil to the eye, frequent and gentle eyelid washing may help. To wash your eyelids:
- Apply a warm washcloth to your eyes. Wet a clean cloth with warm water. Hold the cloth over your eyes for five minutes. Rewet the cloth with warm water when it cools. Gently rub the washcloth over your eyelids — including the base of the eyelashes — to loosen any debris.
- Use a mild soap on your eyelids. Use baby shampoo or another mild soap. Put the cleanser on your clean fingertips and gently massage your closed eyes near the base of your eyelashes. Rinse completely.
-
Source:
https://www.mayoclinic.org/diseases-conditions/dry-eyes/symptoms-causes/syc-20371863
https://www.webmd.com/eye-health/ss/slideshow-dry-eyes
https://www.hopkinsmedicine.org/health/conditions-and-diseases/dry-eye
https://www.health.harvard.edu/a_to_z/dry-eye-syndrome-a-to-z
